

 Now Location:Home--News Center--Industry News
Now Location:Home--News Center--Industry News
On October 19th, the first national platelet gene database collaboration group signing ceremony was grandly opened in Hangzhou, led by the HLA Professional Committee of the China Blood Transfusion Association. 29 provincial-level blood centers and city level central blood stations across the country jointly participated in the signing ceremony of the platelet gene database collaboration group. The conference was lively and grand, bringing a bright red color to October, which was shrouded in the epidemic.
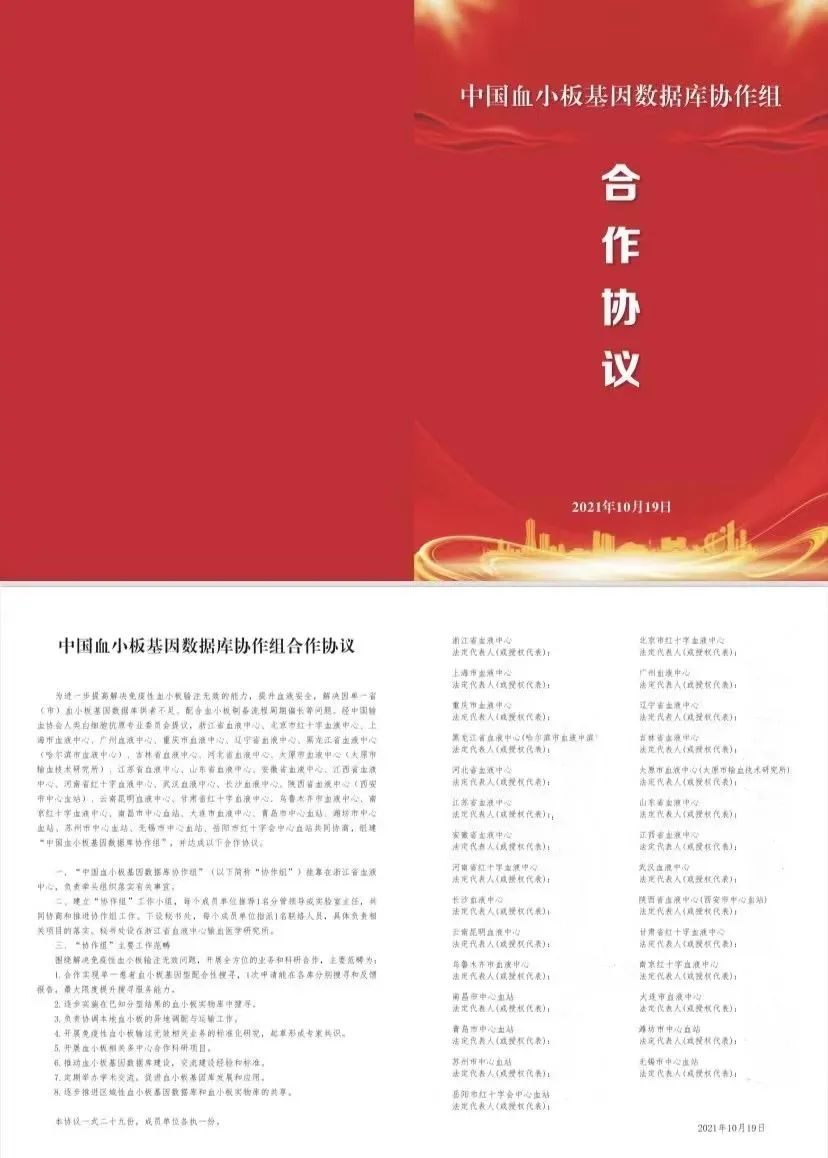
The establishment of the National Platelet Gene Database Collaboration Group this time is another major leap after the provincial platelet alliances. It provides effective support for improving blood safety, solving problems such as insufficient supply of platelet gene databases in a single province (city), and long cycle of platelet preparation processes. It also provides strong support for the precise platelet matching and infusion project promoted by Weihe Biotechnology nationwide. There are a total of 29 provincial and municipal blood centers participating in the collaboration group, among which more than 20 have used HPA combined with HLA-AB typing detection reagents exclusively developed by Weihe Biotechnology for platelet gene bank construction. Based on the number of registered personnel, Weihe's product market share is in an absolute leading position. As an assistant promoter of the construction of the national platelet gene database, the establishment of the national platelet gene database is both an opportunity and a challenge for Weihe. Weihe has also made certain thoughts on the future development direction of platelet precise matching infusion projects:

Future development direction1:
Assist multiple blood centers in carrying out clinical work
Platelet transfusion is an important method for clinical treatment of leukemia, aplastic anemia, tumor radiotherapy and chemotherapy that cause thrombocytopenia or functional abnormalities. The platelet antibodies produced due to the mismatch between HPA and HLA can lead to allogeneic immune thrombocytopenia, which can induce diseases such as ineffective platelet transfusion (PTR), post transfusion thrombocytopenic purpura (PTP), neonatal allogeneic immune thrombocytopenic purpura (NAITP), and also cause related diseases such as transplant rejection in clinical transplantation. Therefore, based on the construction of platelet gene banks in various provincial blood centers, tailored measures will be taken to assist provincial and municipal blood centers in applying platelet gene databases to clinical practice. Two main models will be adopted for clinical use:
1) Platelet transfusion based on HLA and HPA typing
Difficult platelet matching patients: It is recommended that they undergo HLA-I and HPA genotyping, as well as platelet homologous antibody screening to identify antibody properties. They should also search for HLA and HPA matching or antigen level cross reactivity compatible individuals in the platelet donor database, and select suitable platelets based on cross matching.
2) Pre intervention platelet matching
For patients who require long-term platelet transfusion or early bird type patients who may undergo platelet transfusion, it is recommended to first perform HLA and HPA genotyping, in order to screen for platelet transfusion with HPA homology, HLA homology, or HLA cross reactivity group (CREG).
The successful infusion of different matching objects requires collaboration between clinical practice and blood stations. Clinical timely submission of the "Platelet Gene Matching Application Form" to the blood station. The blood center compares and screens platelet donors that match the patient's HPA and HLA typing test results in the existing platelet gene database. 2-3 best donors are identified and recruited, collected, tested, prepared, and distributed in a timely manner Truly achieving the service goal of using platelets as a human resource for the public.
Future development direction2:
Further expand the construction of platelet gene database
Due to the high polymorphism of HLA antigens and the rarity of HPA low-frequency antigens, it is necessary to further expand the construction capacity of platelet gene databases. Some provincial-level blood centers have formed alliances with platelet gene banks across the province, selecting representative demonstration areas to further promote the trial operation of more provincial linkage mechanisms, strengthen the speed of database construction, and increase the probability of local cooperation.
Future development direction3:
Promote the implementation of nationwide platelet off-site allocation
The establishment of the National Platelet Gene Database has achieved data sharing of the National Platelet Gene Database, providing a basis for calculating the distribution frequency of platelet genes in various regions of the country. A linkage mechanism for remote search and coordination has been established to ensure that collaborative units can quickly screen matching platelet data through the database and find matching platelets for patients at the fastest speed. In special circumstances, platelets can also be called from different locations to ensure effective platelet transfusion treatment for patients in the first time, achieving the goal of safe, timely, and effective clinical blood use. Truly promoting the platelet gene bank project, achieving a benign mechanism of having a database to follow, available, and off-site plate retrieval.
From a cost-benefit perspective, it is a trend to establish platelet donor banks in different regions, connect them nationwide, and share resources. As a leading enterprise in providing related products and services, Weihe will further assist blood stations in expanding the construction of platelet gene databases, maintain the bond between blood stations and clinical practice, strengthen communication with clinical doctors, promote the application of platelet coordinated infusion, and achieve precise matching.
