

 Now Location:Home--News Center--Industry News
Now Location:Home--News Center--Industry News
Ankylosing spondylitis is a common rheumatic disease and is becoming increasingly familiar to the public. I believe many patients have heard of HLA-B27, and some even ask a rheumatologist with a test report: "Doctor, look, I found HLA-B27 positive. Do you have ankylosing spondylitis?"
Although everyone knows that HLA-B27 is associated with ankylosing spondylitis, what is HLA-B27? Does HLA-B27 positivity necessarily indicate ankylosing spondylitis? Can ankylosing spondylitis be inherited? Now let's talk about these issues with everyone.
What is HLA-B27?
HLA is the capital prefix of three English words:
H represents human beings(Human)
L represents white blood cells(Leucocyte)
A represents antigen(Antigen)
Human leukocyte antigen (HLA)。
HLA is an individual specific antigen that is genetically controlled on tissue cells. It was first discovered on white blood cells and platelets, but now it has been found that this antigen is widely distributed on the cell membranes of tissues and organs such as the skin, kidneys, spleen, lungs, intestines, and heart.
HLA is the expression product of the major histocompatibility complex (MHC) gene cluster. In the immune system, HLA is mainly responsible for the mutual recognition between cells, inducing immune responses, and regulating immune responses, similar to the identity card of cells, allowing immune cells to identify whether they are "their own people". Once an abnormal identity is detected, the immune response is activated.
The 8th International Organization Compatibility Conference determined that there are 92 HLAs, which belong to the 5 loci A, B, C, D, and DR, respectively called HLA-A, HLA-B, HLA-C, HLA-D, and HLA-DR. There are 42 HLA-B loci, and B27 is one of them.
HLA is a complex identity system of human cells, and each cell carries its own unique type of HLA. HLA-B27 is just one of them, and people with HLA-B27 on their cells are more likely to suffer from ankylosing spondylitis than those without HLA-B27 on their cells.
Does HLA-B27 positivity necessarily lead to ankylosing spondylitis?
Firstly, let me tell you that HLA-B27 positivity does not necessarily indicate ankylosing spondylitis.
On the other hand, it should also be emphasized that HLA-B27 negative cannot rule out the possibility of ankylosing spondylitis.
According to epidemiological investigations, the HLA-B27 positivity rate in patients with ankylosing spondylitis is as high as about 90%, and the HLA-B27 positivity rate in the general population is also 4% to 7%. Therefore, a portion of the general population can also show HLA-B27 positivity.
The incidence rate of ankylosing spondylitis in HLA-B27 positive patients is about 10%~20%, while that in the general population is 1 ‰~2 ‰, a difference of about 100 times. Although HLA-B27 positive individuals are more likely to suffer from ankylosing spondylitis, the probability is not 100%.
Can ankylosing spondylitis be inherited?
More than 50 years ago, people discovered a familial clustering tendency in ankylosing spondylitis. The risk of first-degree relatives (parents, children, brothers and sisters with the same parents) of patients with ankylosing spondylitis is 52-94 times higher than that of the general population. However, with the alienation of kinship with patients, the incidence rate of ankylosing spondylitis rapidly declined.
The onset of ankylosing spondylitis is closely related to genetics. In 1971, researchers found that HLA-B27 was rare among African black people and also rare among African American black people, only found in 4% of African American black people. Approximately half of white American people carried HLA-B27, matched by ankylosing spondylitis, which is also not common among African American people (Baum J. Arthritis Rheum, 1971).
Among patients who have already suffered from ankylosing spondylitis, whether they are African black or European white, the positive rate of HLA-B27 is comparable.
The incidence rate of first-degree relatives of patients with ankylosing spondylitis who are also HLA-B27 positive and HLA-B27 positive is 6-16 times higher than that of the general population with HLA-B27 positive, indicating that in addition to HLA-B27, there are other genetic related factors that affect the incidence of ankylosing spondylitis.
[Extended reading: How HLA-B27 participates in the pathogenesis of ankylosing spondylitis]
Although the relationship between HLA-B27 and ankylosing spondylitis has been confirmed for over 40 years, there is still a long way to go before elucidating its specific mechanisms involved in the pathogenesis of ankylosing spondylitis.
HLA-B27 is an MHC-I class molecule that can present certain pathogenic antigens to induce immune responses in CD8+T cells, but there is currently no confirmed specific "arthritis antigen" that can be presented by HLA-B27.
Another theory suggests that it is not the function of HLA-B27, but the structure of HLA-B27 that causes the disease.
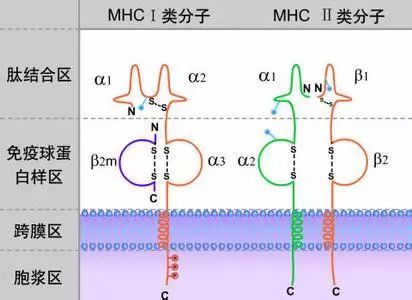
Proteins within cells usually need to be processed and folded in the endoplasmic reticulum to form biologically functional protein molecules. The folded HLA-B27 molecule is composed of heavy chains, β 2-Microglobulin( β A trimer composed of 2m and a short peptide. Compared to other HLA molecules, HLA-B27 has a more unstable structure and is prone to folding errors in the endoplasmic reticulum. The accumulation of misfolded HLA-B27 can cause endoplasmic reticulum stress, activate unfolded protein response (UPR), endoplasmic reticulum related protein degradation (ERAD), and autophagy, inducing many inflammatory factors such as TNF α、 The production of IL1 and IL6.
On the other hand, misfolded HLA-B27 heavy chains are prone to forming dimers, and the expression of HLA-B27 in dimeric state on the cell surface can activate the IL23-IL17 axis, leading to inflammation.
